Medicine, 27.05.2020 07:00 amandasantiago2001
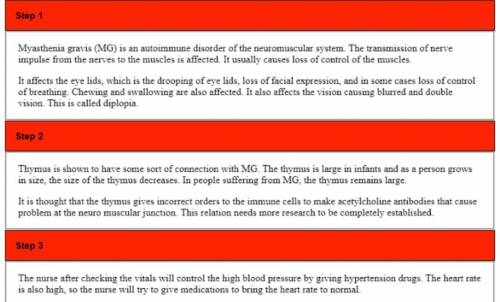
J. B. is a 58-year-old retired postal worker who has been on your floor for several days receiving plasmapheresis qod for myasthenia gravis (MG). Before this admission, he had been relatively healthy. His medical Hx includes HTN controlled with verapamil and glaucoma treated with timolol (ophthalmic preparation). About a year ago, J. B. started experiencing difficulty chewing and swallowing, diplopia, and slurring of speech, at which time he was placed on pyridostigmine (Mestinon). Recently J. B. was diagnosed with a sinus infection and treated with ciprofloxacin. On admission, J. B. was unable to bear any weight or take fluids through a straw. There have been periods of exacerbation and remission since admission. You note that the nursing assistive personnel (NAP) has just entered these vital signs into J. B.'s record. What is your immediate concern and why?

Answers: 2
Another question on Medicine

Medicine, 03.07.2019 20:30
What is the solution of 5/2x - 7 = 3/4x + 14 ? a. x = -6 b. x = 6 c. x= 8 d. x = 12
Answers: 1


Medicine, 09.07.2019 20:10
Mrs. h, age 42 years, is experiencing severe rheumatoid arthritis in her wrists, fingers, and knees. the joints are quite inflamed, red, and swollen. she is sitting rigidly in a chair and refuses to put on a sweater, even though she is shivering, or let anyone touch her arms. she has been prescribed an analgesic and an anti-inflammatory drug, but her dose is not due for another hour. she is feeling nauseated, so she has not eaten for the past 8 hours. based on patient history and the signs and symptoms, discuss how the effects of pain are exacerbating her condition.
Answers: 1

Medicine, 09.07.2019 20:10
Rita schmidt, 74 years of age, is a female patient who was admitted to the surgical unit after undergoing removal of a section of the colon for colorectal cancer. the patient does not have a colostomy. the patient has several small abdominal incisions and a clear dressing over each site. the incisions are well approximated and the staples are dry and intact. there is a jackson-pratt drain intact with minimal serous sanguineous drainage present. the patient has a salem sump tube connected to low continuous wall suction that is draining a small amount of brown liquid. the patient has no bowel sounds. the foley catheter has a small amount of dark amber-colored urine without sediments. the patient has sequential compression device (scd) in place. the nurse performs an assessment and that the patient's breath sounds are decreased bilaterally in the bases and the patient has inspiratory crackles. the patient's cardiac assessment is within normal limits. the patient is receiving o2 at 2 l per nasal hg; heart rate 110 bpm; respiratory rate 16 breaths/min; and the patient is afebrile. the patient is confused as to place and time. cannula with a pulse oximetry reading of 95%. the vital signs include: blood pressure, 100/50 mm. a. explain the assessment parameters used to provide clues to detect postoperative problems early and the interventions needed. b. what gerontological postoperative considerations should the nurse make?
Answers: 3
You know the right answer?
J. B. is a 58-year-old retired postal worker who has been on your floor for several days receiving p...
Questions

Geography, 05.02.2020 11:59

Business, 05.02.2020 11:59

Social Studies, 05.02.2020 11:59


Computers and Technology, 05.02.2020 11:59



Mathematics, 05.02.2020 11:59




Mathematics, 05.02.2020 11:59

Mathematics, 05.02.2020 11:59



History, 05.02.2020 11:59

Mathematics, 05.02.2020 11:59


History, 05.02.2020 11:59